Quality
Quality
Limiting English Proficiency in Ophthalmology (Shark Tank Finalist)
Understanding and Improving the Healthcare Experience for Spanish Speaking Patients with Limited English Proficiency in Ophthalmology
Limited English Proficiency (LEP) patients have been shown to report poor communication with their provider, receive lower quality of care, have higher rates of misdiagnoses, and have significantly more emergency department visits and rehospitalizations. There have been a few studies in ophthalmology showing that there are language related disparities in eye care that must be addressed to achieve health equity and prevent irreversible vision loss.
Project Goal/Improvement/Innovation:
1.) Understand provider and staff satisfaction, challenges, and barriers with providing care for Spanish speaking patients with LEP
2.) Understand patient satisfaction, challenges, and barriers, with their journey in ophthalmology being LEP and with the use of professional interpreter services.
Project Impact:
Our goal through conducting patient, provider, and staff semi structured interviews and observations is to find possible solutions to improving the care of Spanish speaking patients with LEP. After English, Spanish is the second most frequently used language by our patient population at UI Health.
Final Outcomes & Highlights:
From our interviews and observations with providers, staff, and LEP patients, we were able to identify key themes to address in the next steps of our project.
Key Themes were centered around the following:
Provider & Staff Training/Resources
- Providers felt they were not properly trained on how to care for patients with limited English proficiency
- Providers at times use ad hoc interpreters to communicate with LEP patients
- Providers bridge language gaps with non-professional translation tools (e.g. Google Translate)
Difficulty with Communication
- Phone-based interpreters at times may provide flawed translation: omitting details, summarizing, or altering meaning.
- The quality and approach of phone-based translations varies greatly between clinical encounters.
- Patients and providers are often unaware of when a misinterpretation occurs within the clinical encounter.
Issues with Identification
- Patients have no formal mechanism of identifying Spanish speaking staff when arriving to the Illinois Eye & Ear Infirmary
- New LEP patients are often first identified by technicians, not during check-in
Rapport & Trust Building
- Non-verbal communication is often lost even with the usage of a professional interpreter.
- Rapport and trust building between providers and patients are observed to be harder amongst the LEP population.
- Non-bilingual providers were less likely to engage in non-clinical related discussion with Spanish speaking LEP patients compared to English speaking patients
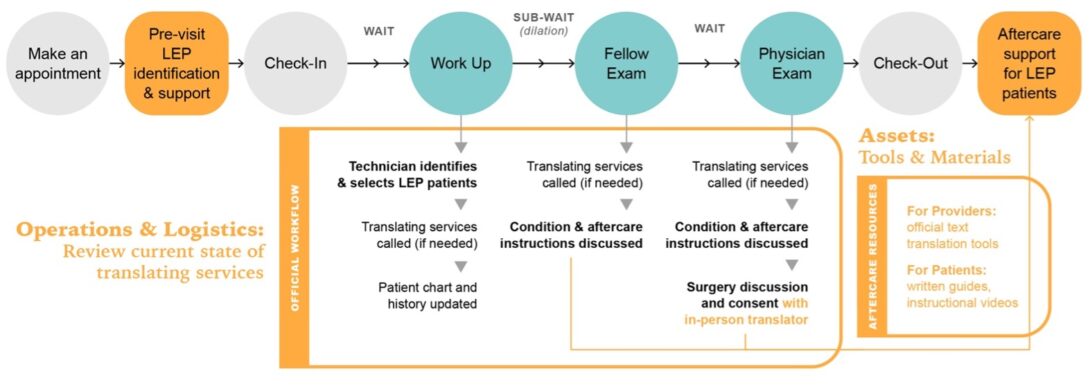
Since this was a pilot study we identified success through insights obtained throughout our interviews and observations with providers, staff, and patients. We were able to create a road map that targets challenges throughout the patient journey that could be improved for providers, staff, and LEP patients (Figure 1).
Operating Room Safety (Shark Tank Finalist)
Operating Room Safety and Communication Project
Key Activities:
- Development and Implementation of Peri-Operative Handoff for Patients in the Neonatal Intensive Care Unit (NICU) and Special Care Unit (SCN) using the Institute for Healthcare Improvement (IHI) Model for Improvement and Kotters Change Principles.
- Train five individuals in basic quality and safety principles (Essentials in Quality and Safety for Clinicians, Graduate Programs in Patient Safety Leadership).
Proposed Outcome(s):
- Reduction in communication related adverse events for surgical patients in the NICU & SCN by implementation of a standardized peri-operative hand off tool.
Metrics:
- Measures identified by multidisciplinary group:
- Process :Compliance with use of the standardized hand off tool before and after surgery
- Outcome: Adverse events related to per-operative hand offs for surgical patients from NICU/SCN
- Balance: Time burden on staff for use of this tool.
Occupational Therapy (OT)
OT 3D Printing Project
Working with the underserved population in Chicago, access to many medical/adaptive equipment can be difficult and quite costly to obtain. Through the Health Equity Pilot Program (HEPP) funding, the Occupational Therapy (OT) department at UIH has been able to purchase a 3D printer and provide patients with free, 3D printed adaptive equipment to increase independence and maximize return to daily life. To date, the OT team has provided patients with 3D printed adaptive utensils, doorknob handles, custom power wheelchair joysticks and varying equipment geared towards maximizing return to self-identified activities of daily living (ADL’s).
Emergency Department
Accelerated Chest Pain Project
The Accelerated Chest Pain Evaluation Task Force is dedicated to identifying the characteristics of urgent and emergent chest pain evaluations at UI Health with a focus on uncovering racial, ethnic, and gender disparities. In May 2022, UI Health implemented an emergency department evaluation pathway to improve and accelerate clinicians’ ability to accurately evaluate chest pain. We are acutely focused on making sure patients of all backgrounds at risk for heart disease – but not today having a heart attack – are receiving appropriate, equitable care and follow-up.
Thus far we have quantified care patterns for 10,000 patients presenting to the UIH emergency department with chest pain over the last 2 years. We have identified potential implementation gaps in the accelerated chest pain evaluation and are working with the emergency medicine, cardiology, internal medicine, and pathology divisions to further hone our use of these new tools.
Department of Ophthalmology/Family and Community Medicine Clinic
Diabetic Retinopathy Project
Diabetic retinopathy is a common eye condition that can lead to vision loss and blindness in people with diabetes. Many patients with diabetes in UI Health’s coverage area don’t receive recommended yearly eye exams.
To combat this problem, the Department of Ophthalmology and the Family and Community Medicine Clinic at UI Health partnered the Institute for Healthcare Delivery Design at UIC to plan and introduce diabetic retinopathy screening at Family Medicine using artificial intelligence technology. The project resulted in clinic screening workflows, patient and provider education materials, and scripts and protocols for clinical staff to carry out the screening service and support patient follow-up visits in Ophthalmology for comprehensive treatment and care. This project is ongoing and is expanding to the Diabetes and Endocrinology Center at UI Health.
Urology
Video-based Education: How Nurse-led Collaboration, Innovation is Improving Prostatectomy Patients’ Self-Management of Indwelling Urinary Catheters
Patients being able to efficiently participate in complicated disease management and self-care activities is strongly associated with improved outcomes, patient satisfaction and health literacy. Frequently, patients are being discharged from same-day surgeries with limited time constraints to provide essential education coupled with the side-effects of recovery from anesthesia. Prostatectomy patients are at a higher risk of developing urinary tract infection (UTI) because of being discharged with a short-term indwelling urinary catheter for 7–10 days after surgery.
Data obtained from the National Surgical Quality Improvement Program (NSQIP), concluded that the prostatectomy patients at UI Health had a higher incidence of UTI in 2021. The primary objective of this quality improvement project was to implement a video-based education discharge tool on short-term indwelling catheter care after Prostatectomy surgery.
Two 15-minute videos were produced with Mariusz Kosla, the Clinical Nurse Consultant II from 5 East, providing hands on demonstration and Susan “Jerri” Klecki, Clinical Nurse Consultant II Perioperative Services, and Marcelo Rodriguez providing the voiceover in English and Spanish, respectively. Additionally, the team developed a flyer containing QR code access to the videos and a standardized “yellow” discharge bag that contains all the needed supplies to care for their indwelling catheter at home. The videos are shown to the patients and caregivers prior to being discharged from the PACU. Currently, the videos have been viewed nearly 400 times on our UI Health YouTube channel.
Sub Epidermal (SEM) Scanner Health Equity Project
Project Problem:
In 2022, 68% of all Patients who developed hospital acquired pressure injuries at UIH for all anatomical locations were in patients with darkly pigmented skin. 51% of these patients had pressure injuries of the sacrococcygeal heels. Of the sacrococcygeal and heel pressure injuries in patients with darkly pigmented skin, 34% were categorized as severe pressure injuries (Stage 3, Stage 4 and unstageable).
Project Outcomes:
In August 2022, The SEM Scanner was evaluated on 6WMICU and 8W Surg/Onc units which have historically been determined to have the highest prevalence of hospital acquired pressure injuries. The trial lasted approximately seven weeks. 346 patients were included in the evaluation and approximately 1789 scans were performed. Approximately 25% of all patients scanned on admission were previously not identified as being at risk based on current risk assessment models. This resulted in significant changes in clinical decision making and the expedient introduction of pressure injury prevention interventions.
Project Impact:
There was a cultural shift in skin assessment with the scanning becoming an integral part of the admission procedure and expediently identifying patients who would previously not be seen as being at risk for breakdown.
The integration of the technology as an adjunct to current practice promoted equitable skin assessment and expedited prevention interventions for all, leading to zero hospital acquired pressure injuries during the evaluation period.
Likelihood to results in meaningful improvement of clinical care:
The project identified that many patients identified as low risk for PI development using the current subjective risk assessment tools (Braden and visual skin assessment) had elevated sacral and heel Delta Values on admission. This established objective early identification of PI risk and led to expedited prevention measures.
Individuals from racial/ethnic minority backgrounds have disparately lower rates of bariatric surgery treatment despite high rates of severe obesity.